

Depression. A word often spoken yet frequently misunderstood. It is more than just feeling sad or having a bad day; it is a pervasive, life-altering condition that affects millions of people worldwide, touching every facet of their lives, from relationships and careers to their very sense of self-worth. Despite its existence, stigma and misconceptions continue to surround depression, leaving many to suffer in silence.
In this post of my Mental Health Series, I delve into the depths of depression, its causes, symptoms, and far-reaching impacts. Through raw and emotional exploration, I aim to demystify this complex condition, challenge the stigmas that often shroud it, and empower readers with tools for both understanding and supporting recovery.


Recovery is not a linear journey; it is a process of navigating setbacks and celebrating progress. Whether you are someone grappling with depression, a loved one offering support, or an organisation looking to create a culture of care, this post is for you. Together, let us move beyond misconceptions, embrace compassion, and learn how we can all contribute to recovery and resilience.
Let us begin this conversation; a conversation that could change lives, and perhaps, even save them.
Depression remains one of the most misunderstood and stigmatised mental health conditions. Many equate it with temporary sadness or laziness, yet it is far more complex; a multifaceted condition that permeates every aspect of a person’s life. To truly understand depression, we must move beyond oversimplified stereotypes and recognise its profound impact on mind, body, and soul.
Depression, also known as major depressive disorder (MDD), is a serious mental health condition. It goes beyond occasional feelings of sadness or low mood. It is a persistent and pervasive state that affects how individuals think, feel, and function in their daily lives.
What makes depression particularly devastating is its ability to distort a person’s perception of themselves and the world, often leading them to feel isolated or ashamed of their condition.
Depression appears differently from person to person. It is not a one-size-fits-all condition, and its diversity underscores the importance of a tailored approach to treatment. Some of the most recognised types:
Each type of depression has its own triggers, challenges, and treatment pathways, making it essential to understand these challenges when supporting someone with depression.
Depression is more than an emotional or psychological issue. It is deeply rooted in the brain’s biological and chemical processes. Studies reveal that depression is linked to imbalances in neurotransmitters, such as serotonin and dopamine, and changes in the brain’s structure and function. But biology alone does not paint the full picture.
Environmental factors, personal experiences, genetics, and societal pressures often converge, creating a perfect storm. For example:
These scenarios highlight the intricate interplay between external circumstances and internal vulnerabilities, further complicating the condition.

Recognising depression as a medical condition is vital. It is not a weakness or a choice. The normal approach and dialect must shift from “Why are you like this?” to “How can we help?” By doing so, we can pave the way for compassion, understanding, and effective support.
Depression is a complex condition that arises from an interplay of various factors. It is not a singular cause-and-effect scenario but rather a combination of biological, psychological, social, and environmental elements. Understanding these causes is essential for addressing the condition with empathy and informed support.
Depression often does not stem from a single cause but rather a convergence of these elements. For example, someone with a genetic predisposition might face a triggering event, such as job loss, compounded by the absence of a supportive social network. This cross-play/interplay creates a personalised journey into depression, highlighting the need for equally personalised recovery strategies.
One common misconception is that depression has a singular, easily identifiable cause. This oversimplification invalidates the lived experiences of many who struggle with the condition. By acknowledging its complexity, we build a deeper understanding and compassion for those affected.
Depression is most definitely a maze of factors that paints a comprehensive, but personalised picture of human vulnerability and resilience. Recognising its variety of causes is the first step in dismantling stigma and creating unique pathways to recovery.
Depression casts a shadow over every aspect of a person’s life. Its effects ripple outward, influencing not just the individual but also their families, workplaces, and communities. The far-reaching impacts of this condition highlight the urgent need for understanding, compassion, and action.


Depression often goes unseen, its impacts masked by the stigma that surrounds mental health. This silence only amplifies its effects, as individuals may delay seeking help or feel unsupported in their struggles.
Recognising the profound impact of depression is not just about statistics; it is about human lives. Every absentee day, strained relationship, or missed opportunity reflects a person battling a condition that is as real and debilitating as any physical illness.
By understanding the multitude impacts of depression, we take a critical step toward creating a world where help is accessible, stigma is eliminated, and recovery becomes a collective effort.
Depression often hides in plain sight, cloaked in everyday behaviours or changes so gradual they blend into the fabric of life. Spotting the signs is not just about observation, it is about curiosity, compassion, and understanding the myriad ways depression can manifest. Each story, symptom, and experience is unique, and this section approaches the signs of depression with the same individuality and depth, recognising its nuanced presence in diverse lives.
Depression often starts by robbing people the joy they once found in life. Hobbies, passions, and relationships that used to bring happiness may now feel burdensome or irrelevant. It is not laziness or apathy, it is the brain struggling to process pleasure.
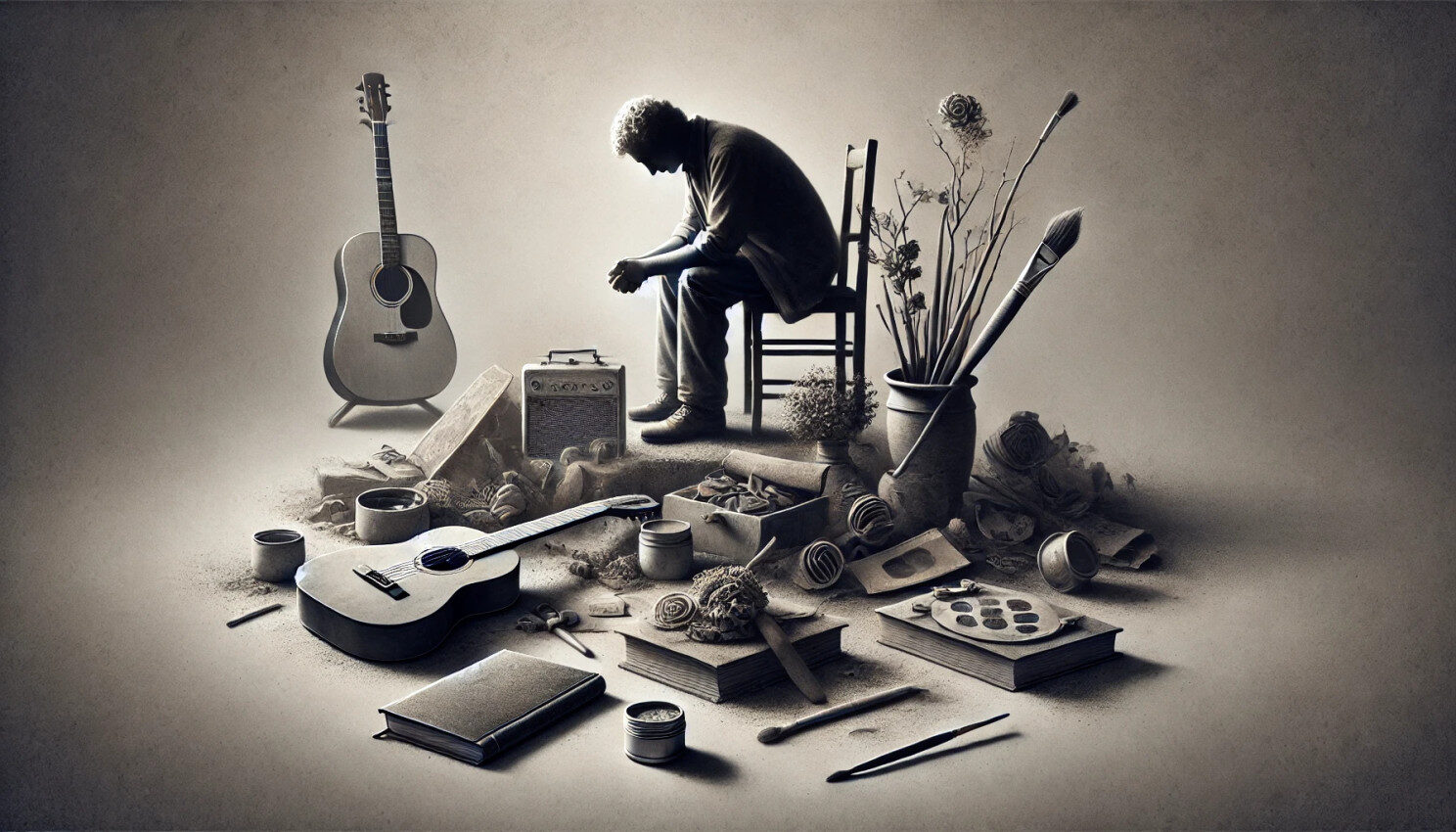

This loss of interest is one of depression’s most telling signs, a shift that signals something deeper than a temporary mood change. When a person withdraws from activities they once loved, it is a silent cry for help that should never be ignored.
Cognitive changes are another hallmark of depression. Difficulty concentrating, indecision, and forgetfulness can disrupt daily life and make even simple tasks seem overwhelming. These signs often manifest in professional and personal settings, such as missing deadlines, forgetting important dates, or struggling with decisions.
Depression clouds the mind, making it hard to process information and maintain mental clarity, often leading individuals to feel frustrated and disconnected from themselves and others.
Depression’s effects are not confined to the mind, it has a profound impact on the body as well. Unexplained aches and pains, chronic fatigue, changes in appetite, and sleep disturbances are common physical symptoms. These issues often persist despite medical tests showing no underlying physical cause, highlighting the intricate connection between mental and physical health.
Recognising these physical signs as potential indicators of depression is crucial, especially when they appear alongside emotional or cognitive changes.
One of depression’s most deceptive traits is its ability to hide behind a mask of normality. Many people with depression maintain a strong outward appearance, excelling at work or socialising while internally struggling. This is particularly common in high-functioning depression, where outward success conceals inner turmoil. It is a reminder that outward appearances can be misleading, and checking in on even the seemingly “strongest” individuals is vital.
Depression does not always appear as sadness. For some, it manifests as irritability, anger, or emotional withdrawal. These behaviours often strain relationships, creating a cycle of isolation and misunderstanding.


Recognising these signs as potential indicators of depression, rather than personality flaws, can lead to more compassionate interactions and early support.
Understanding and recognising the signs of depression is about more than awareness; it is about promoting an environment where individuals feel safe to express their struggles. Every sign is an opportunity to intervene, offer support, and potentially change the trajectory of someone’s life. Depression thrives in silence, but through awareness and action, you can help break the barriers it creates.
Supporting someone with depression is an act of profound compassion, requiring sensitivity, understanding, and action. Depression, often likened to a heavy fog or an endless abyss, has the power to eclipse joy, energy, and hope. For those stepping into a supportive role, understanding the weight of this condition and the transformative impact of their actions is paramount.
Depression affects individuals in deeply personal ways, and no two experiences are identical. Some may withdraw, struggling to find meaning or energy in their daily lives, while others may mask their pain, functioning outwardly but battling an invisible war internally. For supporters, recognising these challenges is essential. This is not about fixing someone; it is about walking beside them, offering reassurance that they are not alone in their struggle.
Mental Health First Aiders (MHFA) are often the first line of defence against the engulfing tide of depression, particularly in workplaces. Their presence demonstrates a commitment to mental well-being, providing an accessible and empathetic resource for those in need.
Supporting someone with depression goes beyond listening; it involves intentional and compassionate actions that acknowledge their humanity and needs:
Depression may feel isolating, but with collective efforts from loved ones, professionals, and MHFAs, individuals can find their way toward light and healing. MHFAs exemplify the belief that no one should face their struggles alone. By building bridges of understanding and compassion, they make recovery possible, one conversation at a time.
Recovery is a Journey, Not a Destination
Recovery from depression is not a straight line; it is a deeply personal journey that ebbs and flows – remember the sign-wave from an earlier post?. It requires time, patience, and unwavering resilience. For some people, it might be a long climb out of a deep, dark well, while for others, it is a series of steps taken in the shadow of ongoing challenges. Depression is not a one-size-fits-all condition, and neither is recovery. Recognising the diversity of this journey is paramount to offering meaningful support.


A journey often begins with acknowledgment. Accepting that depression is present and seeking help takes tremendous courage. For many, this can be the most challenging step, burdened by stigma and feelings of vulnerability. But once this hurdle is crossed, the path to recovery becomes highlighted with possibility.
Professional support, whether through therapy, medication, or a combination of both, plays a crucial role. Cognitive Behavioural Therapy (CBT), mindfulness practices, and newer treatments like Transcranial Magnetic Stimulation (TMS) are examples of how recovery can be tailored to an individual’s needs. But recovery is also about the small wins: getting out of bed, seeking sunlight, or sharing an honest conversation.
Support networks, both formal and informal, are critical during recovery. Mental Health First Aiders (MHFAs), trusted colleagues, friends, and family members can all serve as anchors in turbulent times. Simple acts, such as listening without judgment or accompanying someone to a therapy session, can make an immeasurable difference.
Organisations that promote an environment of care often see the most progress in their workforce’s mental health. Supportive policies, accessible mental health resources, and regular check-ins can help those recovering from depression feel seen and valued.
The journey of a person’s recovery is often bolstered by the right resources. In the UK, individuals can access a wide range of services and support:
Recovery is not just about external help; it is also about inner work. Self-compassion is the cornerstone of healing. Learning to forgive oneself for the perceived failures that depression often magnifies can be liberating. It is okay to stumble, to have bad days, and to feel overwhelmed; what matters is finding the strength to keep moving forward.


Daily practices such as journaling, yoga, meditation, or even spending time in nature can help rebuild a connection to oneself. Recovery is not about erasing depression; it is about learning to live with it in a way that allows for joy, hope, and purpose to re-enter life.
For many, recovery from depression does not signify the end of the struggle but the beginning of a new way of living. It is about building resilience, recognising triggers, and creating a life that supports mental well-being. Recovery is deeply transformative, reshaping how individuals view themselves and the world. Whether you are on the path to recovery, supporting someone else, or striving to foster understanding. Together, through education, empathy, and action, you can illuminate the path out of darkness and into a brighter future.
Stigma is one of the most significant barriers to addressing depression. It silences individuals, fuels misconceptions, and prevents people from seeking help when they need it most. For centuries, mental health conditions like depression have been shrouded in shame, often dismissed as weaknesses or personal failures. These perceptions not only undermine the gravity of the condition but also deepen the suffering of those affected.
View this impacting video here: I had a black dog, his name was depression
To address stigma, society must first confront its misconceptions. Depression is not a choice, a fleeting mood, or a character flaw; it is a legitimate medical condition that deserves empathy and understanding. Education is key to dismantling the falsehoods that perpetuate stigma. Sharing facts, statistics, and real-life stories can pave the way for more compassionate conversations.
Schools, communities, and workplaces must also play a role. Policies that prioritise mental health, open dialogues about mental illness, and celebrate those who seek help can lead the charge in breaking down barriers. Mental Health First Aiders (MHFAs) are instrumental in this shift, serving as champions of empathy and advocates for change.
While addressing stigma is critical, so is fostering hope. Depression can feel insurmountable, but recovery is always possible. Every individual struggling with depression deserves to hear that their story is not over, that help exists, and that brighter days are within reach. Hope begins with small acts of kindness, whether it is a supportive word, a listening ear, or a simple acknowledgment of someone’s pain.
Workplaces can become beacons of hope by creating environments where individuals feel safe to share their struggles and triumphs. Support networks, peer groups, and accessible resources reinforce the message that no one is alone in their battle with depression.

This series has been dedicated to unravelling the complexities of mental health and the barriers that often accompany it. Depression, like so many other mental health challenges, is a condition that requires understanding, compassion, and action. By addressing stigma, fostering hope, and ensuring access to resources, we can collectively shift the narrative around mental health.

This conclusion does not mark the end, but a beginning for every reader to challenge stigma, support those in need, and be part of a something that transforms how society approaches mental health. Whether you are someone who struggles with depression, a caregiver, an advocate, or simply a curious reader, know that your role in this journey matters.

Microsoft Solution Architect, Senior Project Manager, and Mental Health Advocate