In today’s world, discussions about mental health are more prominent than ever, but a critical misunderstanding often arises, the confusion between mental health and mental illness. These terms are frequently used interchangeably, creating misconceptions that hinder awareness, prevent effective support, and prolong stigma.
This post aims to clarify these distinctions. While mental health refers to the overall state of our emotional, psychological, and social well-being, mental illness describes specific diagnosable conditions such as eating disorders, bipolar disorder, or schizoaffective disorder, which require medical attention and professional care. By understanding these differences, we can foster more inclusive workplaces, support individuals living with mental illness, and normalise conversations about mental health as a shared human experience.
In the previous post in this series – “Understanding Mental Health: From Perception to Reality” – I explored what mental health means and how it fluctuates for everyone. This foundational discussion established mental health as a universal, dynamic state. In this post, I will delve deeper into:
- The critical differences between mental health and mental illness.
- How societal misconceptions about conditions like self-harm, suicide, and eating disorders create barriers to understanding and support.
- Why workplaces need tailored strategies to address both mental health challenges and mental illness under the Equality Act 2010.
- Practical steps for addressing misconceptions to create a culture of clarity, empathy, and action.
While this post introduces topics such as eating disorders and psychosis, future posts will explore these topics in depth, providing detailed insights and strategies. Let us take this important step toward reducing stigma, improving knowledge, and supporting well-being in all its forms.
Table of Contents
- A Snapshot: Mental Health vs Mental Illness at a Glance
- Understanding Mental Illness: Beyond the Labels
- The Scales of Mental Health: A New Perspective
- Societal Misconceptions and Their Real-World Impact
- How Workplaces Can Address Both Mental Health and Mental Illness
- Practical Strategies for Change
- Conclusion: Bridging the Gap Between Perception and Reality
A Snapshot: Mental Health vs Mental Illness at a Glance
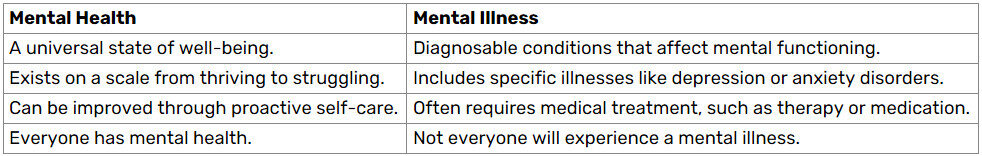
When discussing mental health and mental illness, the terms are often mistakenly treated as the same thing. However, they represent completely different concepts that require clear understanding.
- Mental health refers to a state of well-being that influences how we think, feel, and interact with others. It is universal, everyone has mental health, just as everyone has physical health.
- Mental illness refers to diagnosable conditions that affect mood, thinking, and behaviour, such as depression, anxiety disorders, bipolar disorders, and schizoaffective disorders.
Not everyone will experience mental illness, but many will face challenges to their mental health at some point (and frequently) within their life.
Mental Health in Focus
Mental health is a dynamic state that fluctuates based on life circumstances, environmental factors, and personal practices. For example:
- Thriving Mental Health: A person who feels emotionally balanced, has supportive relationships, and manages stress effectively is said to have good mental health.
- Struggling Mental Health: Periods of high stress, grief, or significant change can cause mental health to dip temporarily, requiring self-care and support to regain balance.
Mental Illness in Focus
Mental illness, on the other hand, involves specific conditions diagnosed by medical professionals. These conditions often have identifiable symptoms and can range in severity. For instance:
- Depression: Persistent feelings of sadness, lack of interest in activities, and changes in sleep or appetite patterns.
- Psychosis: Experiences like hallucinations or delusions that significantly disrupt one’s perception of reality.
- Bipolar Disorder: Episodes of extreme highs (mania) and lows (depression) that affect daily functioning.
- Schizoaffective Disorder: A complex mental health condition that combines symptoms of both schizophrenia (e.g., hallucinations, delusions) and mood disorders (e.g., depression or mania), requiring comprehensive treatment.
A Visual Comparison
To make the distinction clearer, here is a simple snapshot of how mental health and mental illness compare:
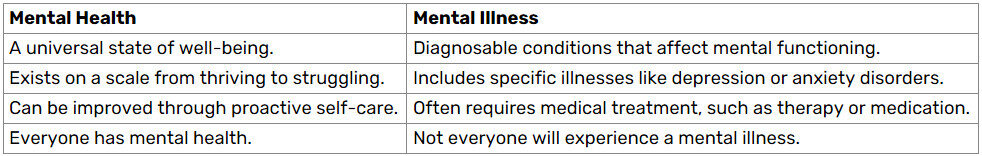
Why This Distinction Matters
Recognising the difference between mental health and mental illness is crucial for several reasons:
- Breaking Stigma: Misusing these terms contributes to stigma. For example, equating mental health struggles with mental illness can discourage individuals from seeking help for everyday stress or burnout.
- Appropriate Support: Understanding this distinction ensures that individuals receive the right type of support, whether it is self-care strategies for stress or professional treatment for a mental illness.
- Workplace Relevance: In the workplace, recognising this distinction enables employers to create both general wellness initiatives for all employees and specific accommodations for those with diagnosable conditions protected under the Equality Act 2010.
Understanding Mental Illness: Beyond the Labels
Mental illness is often misunderstood, partly because it is viewed through a lens of taboo stigma and misinformation. Unlike mental health, which fluctuates naturally and is a shared human experience, mental illness refers to diagnosable medical conditions that significantly impact how a person thinks, feels, or behaves.
Mental illnesses are NOT a reflection of weakness or character flaws; they are medical conditions that often require professional diagnosis and treatment, just like physical illnesses.
What Defines a Mental Illness?
A mental illness is characterised by:
- Persistent Symptoms: Conditions like anxiety disorders or schizophrenia are marked by symptoms that persist over weeks, months, or even years.
- Impairment in Functioning: Mental illnesses often disrupt daily activities, work, relationships, and overall quality of life.
- Medical Diagnosis: Conditions such as bipolar disorder, psychosis, or schizoaffective disorder must be diagnosed by qualified professionals, using criteria from manuals like the ICD-11 (International Classification of Diseases).
Examples of Common Mental Illnesses
Here are some examples that illustrate the diversity of mental illnesses:
- Anxiety Disorders: Conditions like Generalised Anxiety Disorder (GAD), Panic Disorder, or Phobias that cause overwhelming and persistent worry or fear.
- Depression: More than feeling sad, depression includes long-term low mood, loss of interest in activities, and physical symptoms like fatigue.
- Eating Disorders: Conditions like anorexia nervosa, bulimia, or binge eating disorder, which involve unhealthy relationships with food and body image.
- Schizoaffective Disorder: A combination of symptoms of schizophrenia (e.g., hallucinations) and mood disorders (e.g., depression or mania).
- Self-Harm and Suicidal Ideation: These are critical aspects of mental illness, often misunderstood as attention-seeking behaviours but indicative of deep emotional pain.
- Psychosis: Experiencing hallucinations, delusions, or disorganised thinking, which profoundly disrupt perception of reality.
Note: In the United Kingdom, mental health professionals diagnose conditions such as bipolar disorder, psychosis, or schizoaffective disorder using the International Classification of Diseases, 11th Revision (ICD-11), developed by the World Health Organization (WHO). The ICD-11 serves as the primary diagnostic tool for mental and physical health conditions in the UK. The ICD-11 is accessible online through the WHO’s official website: ICD-11.
Mental Illness and Stigma
One of the greatest challenges faced by individuals living with mental illness is society based stigma. Misconceptions such as “mental illness makes people dangerous” or “you can just snap out of it” increase (potentially a pinnacle) feelings of isolation and shame, discouraging people from seeking help. This stigma often stems from a lack of understanding and the media’s portrayal of mental illness as something to fear.
Impact of Stigma:
- Delay in Diagnosis and Treatment: Many individuals wait years before seeking help due to fear of judgement.
- Workplace Barriers: Employees with mental illness may avoid disclosing their condition, missing out on reasonable accommodations protected under the Equality Act 2010.
- Social Isolation: Negative stereotypes, fake influencers, trolls, that lead to marginalisation and withdrawal from supportive networks for those affected or seeking help.
The Role of Legislation
In the UK, mental illness is recognised under the Equality Act 2010 as a disability when it has a substantial, long-term impact on a person’s ability to perform everyday activities. This legal protection ensures that individuals with mental illnesses are entitled to reasonable accommodation in the workplace, such as flexible hours, adjustments to workload, or access to counselling services. However, awareness of these rights is often low, and many employees with mental illnesses do not know about the Equality Act 2010, or feel confident advocating for themselves. This highlights the need for better education and training in workplaces to support inclusivity.
Mental illnesses are complex and multifaceted, requiring understanding, empathy, and professional intervention. While this section offers an overview, specific conditions such as eating disorders, self-harm, and suicide will be explored in depth in future posts within this series.
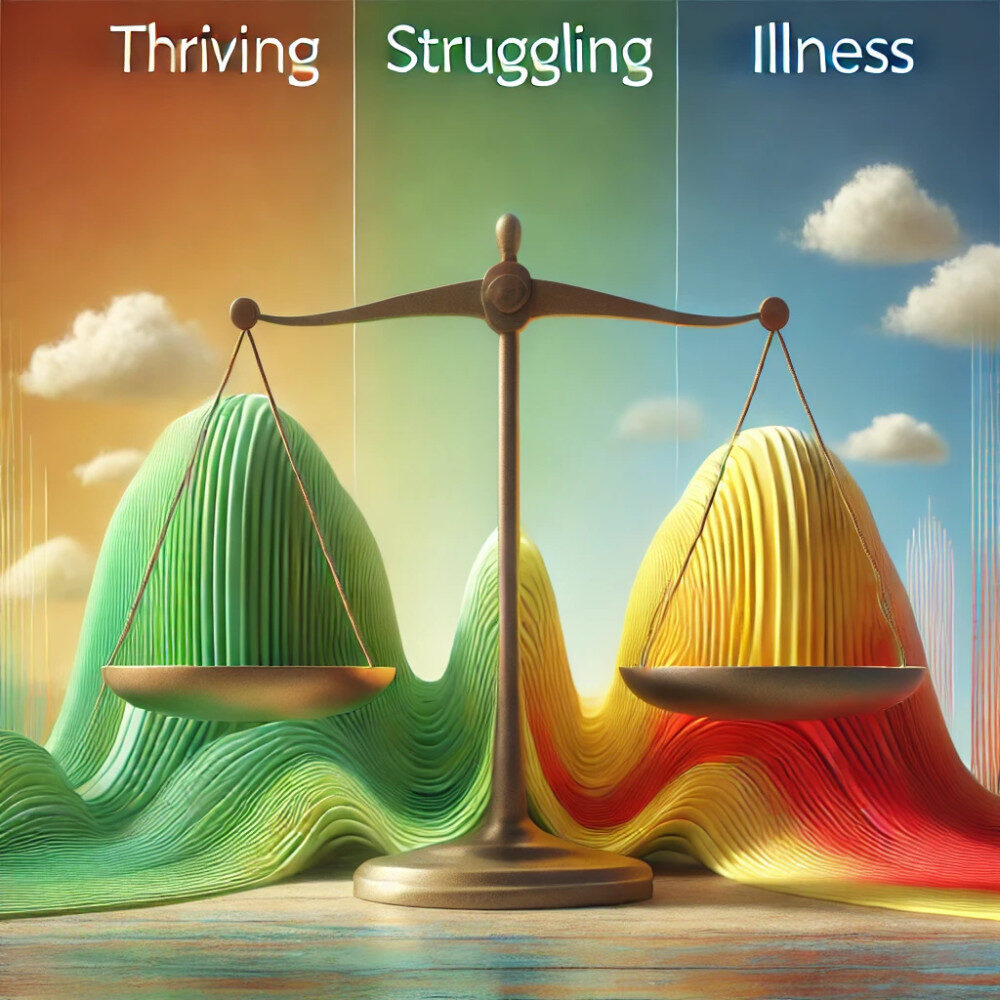
The Scales of Mental Health: A New Perspective
Mental health and mental illness are often viewed as binary concepts – you either have “good mental health” or you are “mentally ill.” However, this perspective oversimplifies the complexity of human mental well-being. A more accurate way to understand mental health is through a set of scales, where individuals move fluidly between thriving, struggling, and living with mental illness depending on various factors such as life circumstances, support systems, and coping mechanisms.
Introducing the Scales of Mental Health
Think of mental health as a balance between various states, much like a set of scales:
- On one side, we have thriving – a state where individuals experience emotional stability, positive relationships, and the ability to manage stress effectively.
- On the other side, we find struggling or illness, which can include temporary challenges such as burnout or diagnosable conditions like depression or anxiety disorders.
These scales are dynamic and ever-changing. For example:
- A person who is generally thriving may temporarily struggle due to grief, workplace stress, or a major life change.
- Conversely, someone managing a diagnosed mental illness may experience periods of stability and high functioning with the right treatment and support.
To help understand this, imagine a horizontal scale divided into three key states:
- Thriving (Positive Mental Health): Emotional well-being is strong. Stress is present but manageable. Individuals feel resilient and supported. Example: Someone who feels motivated at work, enjoys their hobbies, and maintains strong relationships.
- Struggling (Temporary Challenges): Coping abilities are reduced, leading to feelings of overwhelm. Stress may become chronic if not addressed. Example: An employee experiencing burnout due to prolonged work demands or personal loss.
- Illness (Diagnosable Mental Illness Conditions): Includes conditions like bipolar disorder, psychosis, or eating disorders that significantly impair daily functioning. Professional treatment (therapy, medication, or both) is often required. Example: A person with schizophrenia who benefits from regular therapy and support systems.
Key Factors That Shift the Scales
Several factors influence where an individual may fall on these scales:
- Support Systems: Access to a strong support network (friends, family, or professional help) can prevent struggling from escalating into mental illness.
- Life Events: Stressful or traumatic events, such as job loss or bereavement, can tip the balance toward struggling or illness.
- Coping Mechanisms: Healthy strategies like mindfulness, exercise, and self-care can help individuals recalibrate their scales toward thriving.
- Treatment and Recovery: Timely access to professional help, such as cognitive behavioural therapy or medication, enables individuals living with mental illness to manage their symptoms effectively and regain balance.
Why the Scales Matter
Understanding mental health as a set of scales rather than fixed categories has significant benefits:
- Empathy: Recognising that everyone shifts between these states fosters compassion and reduces stigma.
- Early Intervention: Viewing struggling as a temporary state encourages individuals to seek support before challenges escalate into illness.
- Workplace Inclusivity: Employers can better tailor resources to address both general well-being and specific accommodations for employees living with mental illnesses.
I hope this has highlighted the fluid nature of mental health, later posts in the series will explore specific factors in detail. For now, reflect on where you currently sit on your own scales of mental health and consider how external factors influence your balance.
Societal Misconceptions and Their Real-World Impact
Mental health and mental illness are surrounded by societal misconceptions that create barriers to understanding and support. These misunderstandings can elevate stigma, discourage individuals from seeking help, and lead to a lack of appropriate accommodation in both personal and professional settings. Recognising and addressing these misconceptions is essential to fostering a culture of empathy, inclusion, and proactive care.
Common Misconceptions About Mental Health and Mental Illness
- “Mental illness is a choice.” This frames mental illness as a matter of willpower, implying that individuals can simply “snap out of it.” In reality, conditions like depression, anxiety, and bipolar disorder are influenced by complex biological, psychological, and environmental factors.
- “Good mental health means never feeling sad, anxious, or stressed.” Mental health is not about constant happiness. It is about balance and resilience, coping with life’s ups and downs in healthy ways. Feeling stressed or sad is a normal part of the human experience and does not necessarily indicate poor mental health or a mental illness.
- “Mental illness is rare and only affects a few people.” According to Mind UK, 1 in 4 people in England will experience a mental health problem each year. Mental illness is far more common than many realise, and it touches individuals across all demographics, professions, and cultures.
- “People with mental illnesses are dangerous.” This is one of the most damaging misconceptions. Research consistently shows that individuals with mental illnesses are far more likely to be victims of violence than perpetrators.
- “Seeking help is a sign of weakness.” Many people avoid seeking support due to fear of being judged as weak or incapable. On the contrary, reaching out for help demonstrates courage and self-awareness.
The Real-World Impact of Misconceptions
Misconceptions do not just influence individual beliefs, they have tangible consequences for workplaces, communities, and healthcare systems.
- Delay in Diagnosis and Treatment
Stigma and misinformation discourage people from recognising symptoms and seeking help. Many individuals wait years before consulting a professional, leading to worsening conditions and prolonged suffering. Example: A person experiencing early signs of an eating disorder might dismiss their struggles due to societal minimisation of such conditions as “a phase”.
Employees may hesitate to disclose mental health conditions, fearing discrimination or career repercussions. This creates a cycle where issues go unaddressed, potentially leading to burnout or resignation. Employers who fail to understand the distinction between mental health and mental illness risk implementing one-size-fits-all solutions that do not meet the needs of their workforce.
- Marginalisation and Social Isolation
Misconceptions can cause individuals to feel judged, excluded, or misunderstood by peers, family, friends, or colleagues. This lack of social support compounds the challenges of living with a mental illness – being on the end of negative comments can push those seeking help, assurance and confidence deeper down a dark rabbit hole.
Breaking the Cycle of Misconceptions
Addressing these issues requires collective effort across individuals, workplaces, communities, councils, and the government:
- Education: Incorporate mental health awareness into schools, workplaces, and public campaigns to normalise conversations and provide accurate information.
- Representation: Challenge harmful stereotypes in media by advocating for authentic, diverse portrayals of individuals living with mental illness.
- Proactive Policies: Ensure workplaces comply with the Equality Act 2010by creating safe environments for disclosure and implementing reasonable accommodations.
Whilst examining the broad impact of misconceptions, reflect on the misconceptions you may have encountered and consider how you can contribute to changing the narrative around mental health and mental illness.
How Workplaces Can Address Both Mental Health and Mental Illness
The workplace plays a critical role in shaping mental well-being. With most adults spending a significant portion of their lives at work, organisations have a unique opportunity and responsibility to address both mental health and mental illness effectively. However, the distinction between these two concepts often gets blurred, leading to generic policies that fail to meet diverse needs. A delicate approach is essential for creating supportive environments where all employees can thrive, regardless of their mental health status.
Tailoring Workplace Strategies
Workplaces need to adopt a dual-focus strategy that addresses both:
- General Mental Health Initiatives: To promote well-being and prevent mental health struggles.
- Targeted Support for Mental Illness: To accommodate employees living with diagnosable conditions under the Equality Act 2010.

General Mental Health Initiatives
These initiatives aim to create a culture of openness, resilience, and proactive care:
- Wellness Programmes: Offer workshops on stress management, mindfulness, and emotional intelligence. Provide regular communication about the importance of mental well-being.
- Flexible Working Policies: Allow remote or hybrid working arrangements to reduce stress caused by long commutes or rigid schedules.
- Employee Training: Equip employees with the skills to recognise early signs of burnout or mental health struggles, especially for remote workers that attend regular meetings with video technology. Encourage regular check-ins with employees to create a safe space for open conversations. Identify and promote a number of employees to undertake “Mental Health First Aid in the Workplace” (MHFA) training.
- Well-being Resources: Provide access to Employee Assistance Programmes (EAPs) that offer confidential counselling and mental health support. Distribute resources like infographics, guides, or apps focused on self-care and resilience.
Supporting Employees with Mental Illness
For employees living with diagnosable mental illnesses, organisations must move beyond general wellness programmes and implement tailored accommodations:
- Reasonable Adjustments (Equality Act 2010): Examples include flexible hours, reduced workloads during periods of illness, or providing quiet spaces for those with anxiety. Ensure policies are compliant with UK legislation to avoid discrimination claims and promote inclusivity.
- Confidentiality and Trust: Encourage employees to disclose conditions without fear of stigma or career repercussions. Ensure managers, and qualified “Mental Health First Aid in the Workplace” employees maintain confidentiality and offer support based on individual needs. Remember the best action plan – Listening STOPS Distress
- Access to Professional Support: Partner with mental health organisations to provide direct access to therapists or psychiatrists. Create mental health first aider roles within the organisation, empowering employees to offer initial support.
Building a Culture of Inclusion
To truly address mental health and mental illness, organisations must prioritise a culture where employees feel seen, heard, and valued. Here are some ways to embed inclusion into workplace practices:
- Leadership Commitment: Leaders should actively champion mental health initiatives, showing that these efforts are a priority. Share personal stories or examples to normalise conversations around mental health.
- Normalising Conversations: Hold regular events like “Mental Health Awareness Days” or lunchtime talks with mental health advocates. Integrate mental health discussions into performance reviews and team meetings.
- Evaluation and Feedback: Regularly survey employees to assess the effectiveness of mental health policies and initiatives. Use feedback to improve programmes and tailor them to employee needs.

Case Study: A Tailored Approach in Action
Imagine an organisation with a proactive mental health strategy:
- Scenario 1: An employee discloses they are feeling overwhelmed by workplace stress. Their manager arranges a meeting to discuss temporary workload adjustments, provides information about the company’s EAP, and checks in regularly to ensure they are supported.
- Scenario 2: An employee living with bipolar disorder requests flexible hours to manage medical appointments and periods of fatigue. The organisation accommodates this request, ensuring the employee can balance work and health without fear of discrimination.
These examples demonstrate how a tailored approach not only benefits individual employees but also fosters loyalty, retention, and a positive workplace culture.
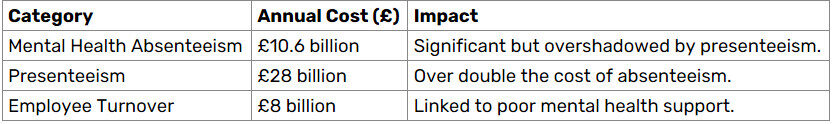
The Business Case for Mental Health
Investing in mental health is not only the right thing to do, it is also a sound business strategy. Addressing mental health challenges can significantly reduce absenteeism, improve employee retention, and enhance an organisation’s reputation.
Reduced Absenteeism
Mental health issues, such as work-related stress, depression, and anxiety, are leading causes of absenteeism in the UK.
- Key Statistic (2022/23): Mental health-related absenteeism directly accounts for approximately £10.6 billion annually (Deloitte, 2022).
- Lost Days: An estimated 17.1 million working dayswere lost due to mental health-related issues in the same period, representing a significant proportion of overall absenteeism in the UK.
Presenteeism: The Hidden Cost
Presenteeism refers to employees attending work despite being mentally or physically unwell, which results in reduced productivity and performance. While harder to measure than absenteeism, its financial impact is much greater.
- Estimated Cost: Mental health-related presenteeism costs UK employers approximately £28 billion annually, more than double the cost of absenteeism.
- Why It Matters: Presenteeism often goes unnoticed, as employees appear “present” but are unable to perform at full capacity. This can include struggling through tasks, making errors, or needing longer periods to complete work.
Improved Retention
Employees who feel supported are more likely to stay with their organisations, reducing the significant costs associated with staff turnover.
- Cost of Employee Turnover: Replacing an employee in the UK costs an average of £30,614, including recruitment, training, and lost productivity. For a mid-sized organisation with 100 resignations annually, this equates to over £3 million in costs.
- Annual Impact on UK Businesses: Staff turnover related to mental health costs UK employers approximately £8 billion annually (Deloitte, 2022).
- Percentage Impact: Employee turnover due to mental health accounts for roughly 36% of total recruitment costs across industries.
Summary of Costs
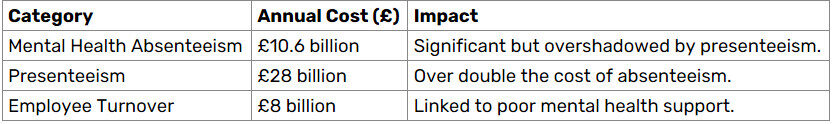
Clarification
- Combined Costs: The total cost of mental health-related challenges to UK employers is estimated at £56 billion annually. This includes absenteeism, presenteeism, and staff turnover combined.
- Breakdown: While absenteeism and turnover are significant contributors, presenteeism is by far the largest factor, accounting for half of the total costs.
Why These Numbers Matter
By proactively addressing mental health:
- Businesses can save billions in avoidable costs.
- Employees benefit from healthier, more supportive work environments, increasing engagement and productivity.
- Organisations gain a competitive advantage by improving retention, reducing absenteeism, and enhancing reputation.
For more insights, refer to:
By proactively addressing mental health, businesses can mitigate substantial costs associated with absenteeism and employee turnover, while fostering a supportive and productive work environment.
Practical Strategies for Change
Addressing mental health and mental illness in workplaces and communities requires actionable steps to break stigma, foster inclusivity, and provide meaningful support. By implementing practical strategies, individuals, organisations, and communities can create environments where mental health is prioritised, and mental illness is addressed with empathy and understanding.
For Individuals
- Educate Yourself: Learn about mental health and mental illness, including common symptoms, challenges, and treatment options. Use reliable sources such as Mind UK or the NHS for accurate information.
- Normalise Conversations: Discuss mental health openly with friends, family, and colleagues. Share your own experiences to create a culture of openness and reduce stigma. Example: Saying, “I’ve felt really overwhelmed lately; I found that talking to someone helped,” can encourage others to seek help without feeling judged.
- Be a Supportive Listener: Practice active listening by being present, showing empathy, and avoiding judgmental responses. Use open-ended questions like, “How are you feeling today?” or “What can I do to support you?”
- Encourage Self-Care: Promote activities like exercise, mindfulness, or spending time outdoors, which support mental health. Lead by example, demonstrating that prioritising self-care is not a luxury but a necessity.

For Workplaces
- Develop Clear Policies: Create or update mental health policies to address both general mental health and specific accommodations for mental illnesses. Ensure compliance with the Equality Act 2010, which protects employees with mental health conditions.
- Provide Training and Awareness: Train managers and teams on how to identify and respond to signs of mental health struggles or illnesses. Include topics such as recognising burnout, supporting employees with anxiety, and reducing stigma. Example: Run events during World Mental Health Day to highlight available resources and share success stories.
- Promote Accessible Support Services: Partner with local organisations to provide free or low-cost counselling, helplines, or peer support groups.
- Offer Comprehensive Resources: Provide access to Employee Assistance Programmes (EAPs), on-site counselling, or mental health helplines. Share educational materials, such as posters or infographics, that explain mental health terms and available support.
- Establish Mental Health First Aiders: Train employees to serve as Mental Health First Aiders (MHFA) who can offer initial support and direct colleagues to professional help.
- Foster a Culture of Openness: Encourage regular check-ins, wellness days, and open-door policies where employees feel comfortable discussing mental health concerns.
Conclusion: Bridging the Gap Between Perception and Reality
Understanding the distinction between mental health and mental illness is not merely an academic exercise, it is a foundational step toward creating workplaces where everyone feels supported, respected, and valued. This awareness allows us to challenge harmful misconceptions, break down barriers, and take meaningful action to support those around us.
Completing the Level 3 Mental Health First Aid in the Workplace course, provided by Qualsafe, has been an eye-opening experience for me. The course reinforced the importance of listening, empathy, and practical action. It introduced an invaluable framework for offering immediate support, encapsulated in the LISTEN S.T.O.P.S. DISTRESS action plan:
- S – Spot signs of distress: Be vigilant in recognising changes in someone’s behaviour or mood.
- T – Talk: Start a conversation by saying what you have noticed and invite the person to share their thoughts. Use empowering messages such as “How are you feeling today?” or “What can I do to support you?”.
- O – Offer care, hope, and comfort: Demonstrate empathy and provide reassurance without judgement.
- P – Professional/Organisation Support: Encourage the individual to seek professional help or access organisational resources, such as counselling or helplines.
- S – Self-help and other strategies: Suggest simple self-care strategies or tools that may help the individual regain balance.
This plan is a practical, compassionate approach that aligns perfectly with the overarching goal of this blog series: to turn understanding into action.
Key Takeaways
- Mental Health vs Mental Illness: Mental health is a universal experience, encompassing emotional, psychological, and social well-being. Mental illness involves diagnosable conditions such as depression, anxiety, psychosis, or eating disorders.
- The Power of Conversations: Encouraging open discussions can help challenge stigma, provide comfort, and guide individuals toward professional support.
- The Role of Workplaces: Tailored strategies, compliance with the Equality Act 2010, and fostering a culture of empathy are vital for inclusive workplaces.
- LISTEN S.T.O.P.S. DISTRESS: This structured action plan offers a clear pathway for supporting someone in need while maintaining their dignity and privacy.
A Call to Action
Understanding mental health is only the beginning; action transforms knowledge into impact. Whether you are an employer, colleague, or friend, you have the power to make a difference by listening without judgement, offering support, and challenging misconceptions.
- Ask yourself: What steps can I take to support mental health in my work and personal spaces?
- Act now: Normalise conversations about mental health. Take a course, such as the Qualsafe Mental Health First Aid in the Workplace, to equip yourself with the skills to make a tangible difference.
We can create a society where mental health and well-being are understood and elevated, and where no one feels left behind – the challenge is ongoing, the results are essential.
Next in the Series
In the next post, “The Role of a Mental Health First Aider“ we will examine the role of a Mental Health First Aider within the Workplace. Join me as we continue this vital journey toward greater understanding and inclusivity.